Exploring Pharmacological Therapies for Fracture Risk Reduction in Adults with Osteogenesis Imperfecta
Month: March 2023
The IMPACT Survey
Living With Osteogenesis IMPerfecta: UnderstAnding Experiences Based On Community InsighT and Evidence Survey, the IMPACT Survey
 What is the IMPACT survey?
What is the IMPACT survey?
In 2021, the Osteogenesis Imperfecta Foundation (OIF), the Osteogenesis Imperfecta Federation Europe (OIFE), and Mereo BioPharma collaborated closely to launch the IMPACT Survey. The goal of this project was to capture and quantify the real impact OI has on the lives of people with OI, their families, and caregivers. We were thrilled that more than 2,200 OI community members from 66 countries participated in this survey!
The survey was based on evidence gaps around:
- Clinical impact of OI on affected individuals
- Humanistic impact on individuals, their families and caregivers
- Economic impact on individuals and wider society
The IMPACT survey is now closed. Thank you to all participants who made this possible.
What were the target groups?
The survey was developed for the following primary target groups:
- Adults with OI (over 17 years old)
- Parents (without OI) of children with OI
- Parents (with OI) of children with OI
- Adolescents with OI (12 – 17 years old)
In addition to the target groups above, there were also a substantial number of responses from
- Parents of adults with OI
- Close relatives of people with OI
There were different questions based on which target group you belong to. Adults with OI who had children with OI, could answer both on behalf of themselves and their children.
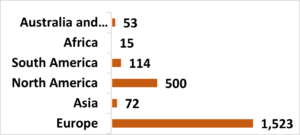
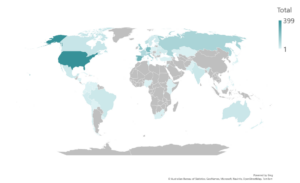
Geographic distribution of respondents
The collaborative survey development allowed members across OI communities and geographies to participate.
What will the data be used for and how will it be stored?
The IMPACT Survey provides a large global dataset describing the experiences of the OI community. The results of this survey are being used to improve healthcare services and potential future treatments for OI.
The data was gathered on a confidential and anonymous basis, with Non-Personally Identifiable Information (Non-PII) . It will be securely stored by Wickenstones according to Data Protection Regulations. The data is now being analyzed according to the plan developed by the Steering Committee, to prepare four proposed central publications on the impact of OI in peer-reviewed, scientific journals.
What data has been published? What are the findings?
So far, the first article “The patient clinical journey and socioeconomic impact of osteogenesis imperfecta: a systematic scoping review” was published in Orphanet Journal of Rare Diseases in February 2023. The purpose of this review was to capture and quantify the published evidence relating specifically to the clinical, humanistic, and economic impact of OI on individuals, their families, and society.
The review suggests that there is limited data regarding health concerns beyond bone health and how these concerns may impact health-related quality of life, in particular that of adult men and other family members.
The four remaining articles will be published in 2023 and 2024.
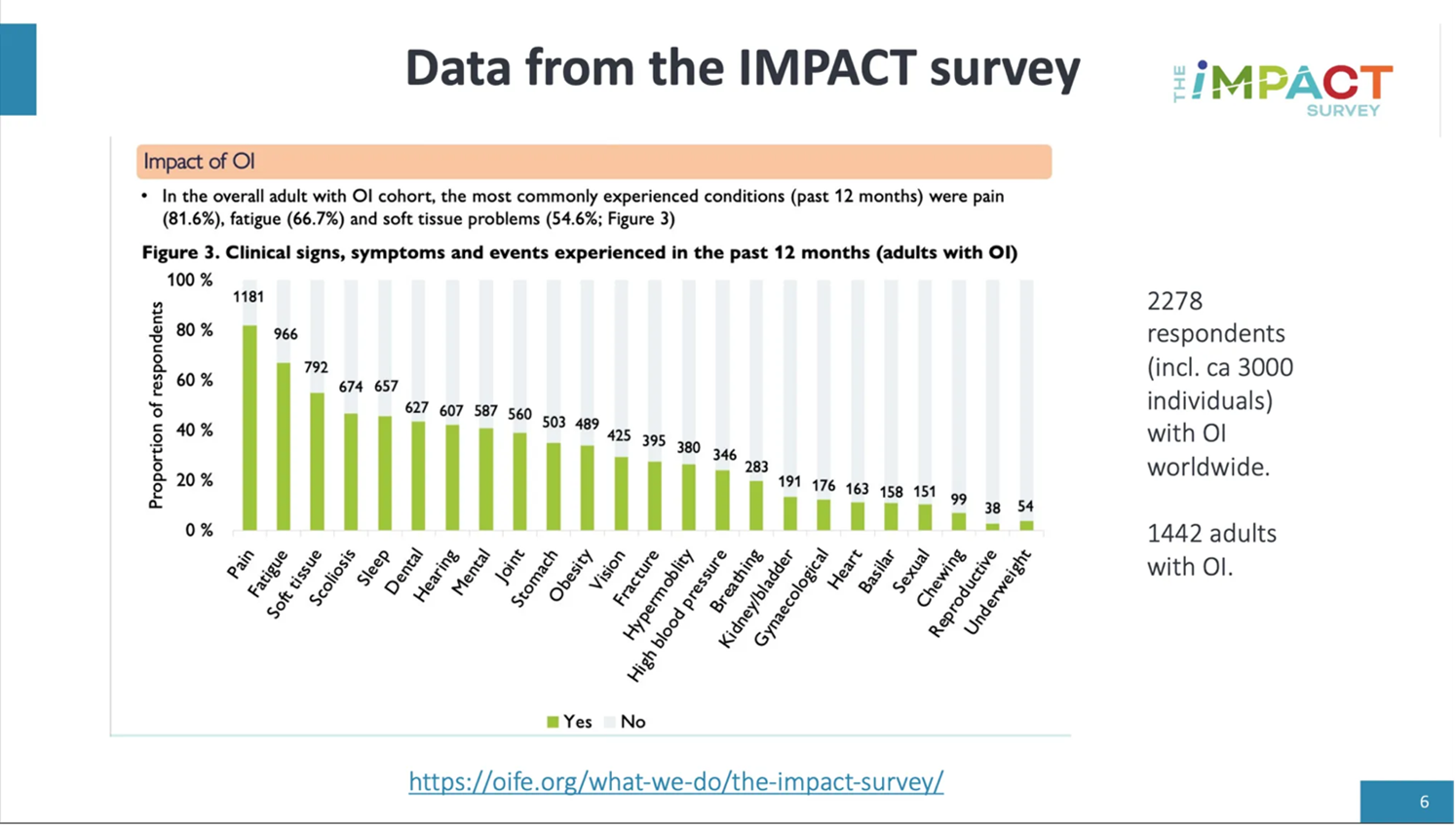
The graphic below describes the most common health conditions in adults with OI (of the past 12-months prior to answering). Pain, fatigue and soft tissue are the most common symptoms, while fractures are in 13th place for the adult population.

We have been given permission to share this graphic.
OIF E-Newsletter: March 2023
The OIF’s March E-Newsletter is here! Click here to read about OIF Membership, an important Medicaid update, the Pain and OI survey, upcoming events, and more.
**Important Medicaid Information!**
During the pandemic, state Medicaid programs were required to keep beneficiaries enrolled, even if they did not meet the eligibility criteria. This requirement will expire on May 11, 2023. With the Public Health Emergency ending, states can resume Medicaid disenrollment starting April 1 – leaving individuals without health coverage. The OIF urges you to contact your state Medicaid agency providers to retain coverage or if no longer eligible switch to other sources of coverage.
The Medicaid and CHIP Communications Toolkit suggests taking the following steps to stay enrolled:
- Update your contact information – Make sure your state’s Medicaid or CHIP program has your current mailing address, phone number, email, or other contact information. This way, they’ll be able to contact you about your Medicaid or CHIP coverage.
- Check your mail – Your state’s Medicaid or CHIP program will mail you a letter about your Medicaid or CHIP coverage. This letter will also let you know if you need to complete a renewal form to see if you still qualify for Medicaid or CHIP.
- Complete your renewal form (if you get one) – Fill out the form and return it to your state’s Medicaid or CHIP program right away to help avoid a gap in your Medicaid or CHIP coverage.
Other important messages:
- If you no longer qualify for Medicaid or CHIP, you may be able to get health coverage through the Health Insurance Marketplace®. Marketplace plans are:
» Affordable. 4 out of 5 enrollees can find plans that cost less than $10 a month.
» Comprehensive. All plans cover things like prescription drugs, doctor visits, urgent care, hospital visits, and more. - Losing Medicaid or CHIP coverage is a Qualifying Life Event (QLE), which allows you to enroll in a Marketplace plan outside of the Open Enrollment Period.
- Visit HealthCare.gov or call the Marketplace Call Center at 1-800-318-2596 (TTY: 1-855-889-4325) to get details about Marketplace coverage.
- If your child no longer qualifies for Medicaid, you may be able to get them health coverage through your state’s Children Health Insurance Program (CHIP).
- For more information about Medicaid renewal or CHIP coverage, contact your state Medicaid office or visit Medicaid.gov.
For more information, please consult: Medicaid.gov/Renewals
For those who will not be covered through Medicaid, please find information on Federally-Facilitated Marketplace (FFM) coverage below:
Federally-Facilitated Marketplace (FFM): Overview of Key FFM Processes and Updates on Plans for Medicaid Unwinding
Medicaid Unwinding Special Enrollment Period (SEP)
- To ensure individuals have sufficient time to enroll in Marketplace coverage during the unwinding period, consumers who lose Medicaid/CHIP coverage between March 31, 2023 and July 31, 2024 will be eligible for a 60-day SEP beginning the day they submit or update a Marketplace application.
- Consumers can access this Unwinding SEP by submitting or updating an application through HealthCare.gov, a certified partner that supports SEPs, or the Marketplace Call Center.
- CMS has published Marketplace guidance on the unwinding SEP: https://www.cms.gov/technical-assistance-resources/temp-sep-unwinding-faq.pdf
- CMS recommends that Medicaid/CHIP enrollees submit or update an application on HealthCare.gov as soon as they receive their Medicaid/CHIP termination letter from their state.
More information can be found at: https://www.healthcare.gov/medicaid-chip/transfer-to-marketplace/