SHARE
Genetics
Osteogenesis imperfecta (OI) is the result of a change in genes that are instructions for making type 1 collagen (the major protein in bone and skin). The change may result in either a decreased amount of type 1 collagen, or cause type 1 collagen to have an abnormal structure/shape. Either of these changes results in weak bones that fracture easily.
How Genes Work
Genes are units of hereditary material (DNA) that tell the cells in our bodies how to make something. We receive two copies of each gene—one from each parent. Most of the time genes function the way they are supposed to. However, genes can sometimes be altered by a change (mutation). Changes in genes can result in either nothing being made from that gene, or can cause the product of the gene to be abnormal in structure or function.
How OI is Inherited
Inheritance is when genetic information is passed from parents to their children. Different types of OI have dominant, recessive, or X-linked inheritance. Dominant inheritance occurs in 90% of individuals, recessive inheritance occurs in 5-10% and X-linked occurs in less than 5%. It is important to have genetic testing to know the genetic defect causing OI for family planning and participation in OI research studies. Learn more about the three types of inheritance below.
 Dominant Inheritance
Dominant Inheritance
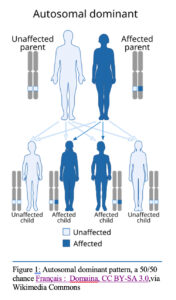
The most prevalent types of OI have dominant inheritance. This means that there is a change in one of the two copies of a gene. About 90% of people diagnosed with OI have a single change in the genes COL1A1, COL1A2, or IFITM5. People can inherit dominant OI from a parent, or they can have a new change in the gene (no family history). About 20-30% of people diagnosed with OI have a new change not inherited from a parent. The new change occurs when a parent’s genes are being copied to put into the sperm or egg cell to pass along to offspring. The changes are an error in copying the gene that results in part of the instructions being left out or misspelled.
Whether inherited from a parent or not, the person with dominant OI can pass OI to their children (50-50 chance in each pregnancy). The affected child of an OI parent has the same gene change as the parent, and generally the same degree of severity (OI type). However, there may be some differences in the child compared to the parent. If the parent with dominant OI passes on his or her normal gene to a child, that child will not have OI and cannot pass on the disorder to his or her own children.
The affected child who has the new dominant gene for OI has a 50 % chance to pass the disorder on to each of his or her children. In addition, unaffected siblings of a person whose dominant OI is caused by a spontaneous mutation have the same risk of having an OI child as the general population.
A special subset of dominant inheritance is Parental Mosaicism. Mosaicism is where some cells in the body have a genetic change (mutation) and other cells do not. This is like a mosaic tile design where some tiles are of one color and some another color but make up a whole picture. People who are “mosaic” may not have a disorder or symptoms, but can have children who do, as the children would have the change (mutation) in all their cells. This is a special instance of dominant inheritance in which the person who has only some cells with the genetic change are not affected with OI but can have affected children.
In OI, a dominant genetic defect causes one of two things to occur:
- The dominant altered gene can cause cells to make a type I collagen protein with an abnormal shape or structure (quality). This type of changes usually causes Type II, III, or IV OI.
- The dominant altered gene does not make any collagen protein. Although some collagen is produced by instructions from the normal gene, only half of the normal amount of collagen produced (decreased quantity); this is typical of Type I OI.
Recessive Inheritance
Most of the rare (non-collagen) types of OI, which are caused by mutations in genes other than the primary collagen genes (COL1A1 and COL1A2), have recessive inheritance. In recessive inheritance, the affected individual has changes in both copies of a particular OI gene. About 5-10% of people diagnosed with OI have a form that is recessively inherited. They have inherited a change in the gene from both parents. The parents are generally not aware they are carriers because they have one normal copy which is sufficient to prevent disease. When a couple has a child with recessive OI, the risk of having additional children with OI is 25% with each pregnancy. The children of affected persons with recessive OI will all be OI-carriers, because they will inherit one of the two mutant gene copies from their affected parent but would not be expected to have OI themselves.
In OI, a recessive genetic defect causes one of two things to occur:
- Disruption in the Function of Proteins Involved in Collagen Processing: In recessive forms of OI, certain gene mutations affect proteins that are essential for collagen modification and stability. When these proteins are defective or absent, the collagen produced is structurally abnormal and less stable. This is characteristic of OI types VII and VIII.
- No Functional Collagen Protein Produced: In more severe cases of recessive OI, mutations in genes result in the complete absence of functional proteins necessary for collagen modifications, which result in an unstable collagen structure. Without these proteins, collagen fibers are improperly formed, or their production is significantly reduced. These mutations result in severe forms of OI, such as type VII.
X-linked Inheritance
One quite rare type of OI is X-linked, which means that the causative gene is on the X-chromosome. Since males have only one X-chromosome, only males will be clinically affected and they would have inherited the change in the MBTPS2 gene from their carrier mother. Most carrier mothers will have no symptoms, but some can have mild symptoms. The daughters of affected males will themselves be carriers, but the sons of affected males would not be at risk for OI greater than the general population.
Navigating OI Care: The Roles of Genetic Counselors and Medical Geneticists
Two key professionals involved in diagnosing and managing OI are genetic counselors and medical geneticists.
Genetic Counselor: Genetic counseling is a medical specialty which deals with the occurrence or risk of recurrence of a genetic disorder in an individual or family. You would typically see a genetic counselor after first getting diagnosed with OI. A genetic counselor is a healthcare professional trained in human genetics and psychosocial counseling that can provide information about how a genetic condition like OI could affect an individual or family and support them in making the best possible adjustment to the diagnosis. Genetic counselors also help order and interpret genetic tests (DNA analysis) that are designed to help estimate the risk of a disease. A genetic counselor can help determine whether a person’s OI was inherited or was the result of a spontaneous variant (mutation) and can help them make an informed decision about their medical situation and family planning1. DNA analysis is useful for assisting in the diagnosis of OI and in family planning decisions.
Medical Geneticist: A medical geneticist is a medical doctor who is an expert in evaluating and managing patients with genetic disorders. For many children and adults with OI, this type of provider is crucial for monitoring and treating their OI, much like the role of a primary care provider for overall management of care. Working with a geneticist can help you better understand your type of OI, its severity, symptoms, and know about potential treatment options that are more appropriate for the kind of OI you have. Geneticists can be an essential part of a multidisciplinary care team and can monitor and manage bone health, and determine whether a variety of treatments, including antiresorptive and anabolic therapies, may be beneficial to address low bone density.
Diagnosing Osteogenesis Imperfecta (OI)
Genetic Diagnosis/Testing
Genetic tests for OI can be conducted through blood or saliva samples from which DNA is then extracted and tested. There are different types of test that a geneticist may order. For people/families with OI who have not had genetic testing, a “panel” that tests multiple OI genes is usually the first step. It is expected in the future that exome or genome sequencing may replace “panel” testing. For cases where the OI gene is known in the family, testing that one specific gene for the specific change seen in the family is typical.
Types of Tests*: (Organized by most general to most specific):
- Whole exome or genome sequencing. Exome sequencing and genome sequencing test all known genes for changes, including both genes related to OI and those not related to OI
- “Osteogenesis Imperfecta” or some other “Bone Fragility Panel” test only OI and bone related genes, both dominant and recessive types. Not all panels include all genes and so the doctor or genetic counselor should check with the laboratory to know what is or is not included.
- COL1A1/COL1A2 genetic testing will detect dominant forms of OI but not recessive types.
How should test results be interpreted?
Genetic laboratories classify changes in genes according to professional laboratory standards. The specific categories of classification are:
- Pathogenic – these are changes in genes known with certainty to cause OI
- Likely Pathogenic – these are changes where most of the evidence indicates that the change causes OI
- Variant of Uncertain Significance (VUS) – these are changes where there is not enough evidence or experience to know if they cause OI or not
- Likely Benign – these are changes that are probably not harmful or not causative of OI
- Benign – these are changes known not to cause OI or other problems
If someone has undergone genetic testing for Osteogenesis Imperfecta (OI) and the test did not report a genetic change in an OI gene, it is important to evaluate what type of test was done before drawing conclusions.
Genetic testing for OI may begin by screening only for dominant mutations in the COL1A1 and COL1A2 genes; however, 5-10% of people with OI have changes in other genes. If the initial genetic test only covered COL1A1 and COL1A2, and the result was not diagnostic, more comprehensive genetic testing, such as a panel of OI genes or exome or genome sequencing may be performed.
If comprehensive genetic testing (exome, genome or OI panel) does not identify a genetic change associated with OI, other diagnoses may be considered. There are several other bone disorders that resemble OI in their symptoms. If genetic testing for OI is negative, it advisable to consider conditions with similar clinical presentations. Please review our Differential Diagnosis fact sheet to find out more information on these disorders.
Clinical Diagnosis
Osteogenesis Imperfecta (OI) is often identified through a combination of clinical signs and a review of the patient’s family history. Key features of OI include frequent bone fractures, often resulting from minor trauma, and bone deformities like bowed legs or scoliosis. Other hallmark signs include a bluish tint to the whites of the eyes (blue sclera), hearing loss, short stature, loose joints, and muscle weakness. A family history of OI or frequent fractures in relatives can be an important indicator, as the condition is often inherited. Healthcare providers will ask about any family members with a history of bone fragility, hearing loss, or short stature, as well as any known OI diagnoses in the family. While clinical characteristics and family history can strongly suggest OI, further testing—such as genetic analysis or bone density scans—is often needed to confirm the diagnosis and rule out other similar conditions.
Genetic versus Clinical Diagnosis of OI
Clinical signs might be appropriate for diagnosing Osteogenesis Imperfecta (OI) in cases where physical characteristics such as recurrent fractures, blue sclerae, dentinogenesis imperfecta, and short stature are prominent, particularly in moderate to severe forms of the disorder. This approach is advantageous in resource-limited settings or when immediate clinical management is necessary. Genetic testing is indicated when an OI diagnosis cannot be made on physical examination, then the course is unusual for OI, or where there are overlaps with other bone disorders, or when a definitive diagnosis is needed for family planning, understanding inheritance patterns, and tailoring treatment plans. It is especially useful in prenatal or early-life settings, where skeletal abnormalities may not yet be fully apparent, allowing for early detection and intervention based on specific gene mutations.
References:
1 Genetic Counseling, National Human Genome Institute, last accessed 06/14/2023, https://www.genome.gov/genetics-glossary/Genetic-Counseling
